Understanding the Effects of Bariatric Surgery on Diabetes Remission and Metabolic Health
Understanding the Effects of Bariatric Surgery on Diabetes Remission and Metabolic Health
Bariatric surgery, also known as weight loss surgery, is a surgical procedure that involves modifying the gastrointestinal tract to induce weight loss in people who are severely obese. Bariatric surgery has been found to be an effective treatment option for obesity-related health conditions, including type 2 diabetes. In fact, studies have shown that bariatric surgery can lead to significant improvements in glucose control, with some patients achieving complete remission of their diabetes. In this article, we will explore the effects of bariatric surgery on diabetes remission and metabolic health.
Types of Bariatric Surgery
There are several types of bariatric surgery, but the most commonly performed procedures are gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Gastric bypass surgery involves rerouting the small intestine to a small stomach pouch, limiting the amount of food that can be eaten and reducing the absorption of calories. Sleeve gastrectomy involves removing a portion of the stomach to create a smaller stomach pouch, limiting the amount of food that can be eaten. Adjustable gastric banding involves placing an inflatable band around the upper part of the stomach to create a smaller stomach pouch.
Effects of Bariatric Surgery on Diabetes Remission
Bariatric surgery has been found to be an effective treatment for type 2 diabetes, with many patients experiencing significant improvements in glucose control and even complete remission of their diabetes. A study published in the New England Journal of Medicine found that 62% of patients who underwent gastric bypass surgery achieved complete remission of their diabetes, compared to only 6% of patients who received conventional medical therapy. Similarly, a study published in JAMA Surgery found that 68% of patients who underwent sleeve gastrectomy achieved complete remission of their diabetes, compared to only 4% of patients who received conventional medical therapy.
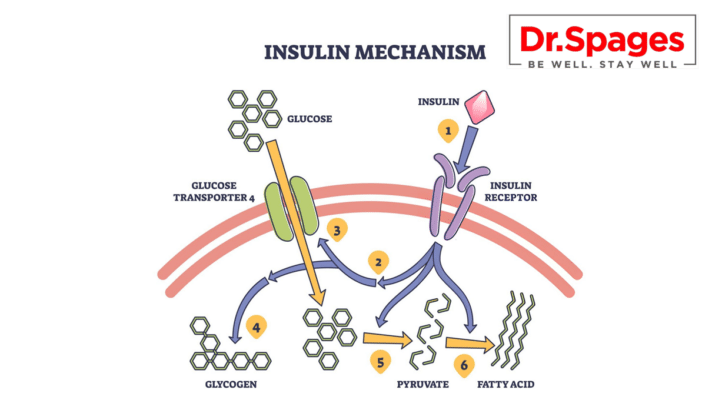
The mechanisms behind the diabetes remission observed after bariatric surgery are not completely understood, but it is believed to be related to changes in gut hormones, particularly glucagon-like peptide-1 (GLP-1) and peptide YY (PYY). These hormones are secreted by the intestines in response to food intake and play a role in regulating glucose metabolism. Bariatric surgery has been found to increase GLP-1 and PYY secretion, which may contribute to improved glucose control and diabetes remission.
Effects of Bariatric Surgery on Metabolic Health
Bariatric surgery has also been found to have significant effects on metabolic health beyond its effects on diabetes remission. In addition to weight loss, bariatric surgery has been found to improve lipid profiles, reduce blood pressure, and improve insulin sensitivity. A study published in Diabetes Care found that patients who underwent bariatric surgery had a greater reduction in HbA1c (a measure of average blood glucose levels) and a greater reduction in cardiovascular risk factors compared to patients who received conventional medical therapy.
Conclusion
Bariatric surgery is an effective treatment option for obesity-related health conditions, including type 2 diabetes. The surgery has been found to lead to significant improvements in glucose control, with some patients achieving complete remission of their diabetes. Bariatric surgery has also been found to have significant effects on metabolic health beyond its effects on diabetes remission, including improvements in lipid profiles, blood pressure, and insulin sensitivity. While bariatric surgery is a major surgical procedure and not without risks, it should be considered as a treatment option for severely obese individuals with type 2 diabetes who have failed to achieve adequate glycemic control with conventional medical therapy.
About Dr Spages
Dr. Jonathan Spages, DC has expertise in Functional Medicine and possesses exceptional abilities to address the underlying issues related to chronic conditions like type II diabetes and hypothyroidism. He doesn’t rely on the traditional practice of prescribing drugs and hormones as the primary solution for these illnesses, as he has transcended the conventional approach.
Dr. Spages uses innovative diagnostic testing and analysis techniques that are seldom performed in the standard medical setting. This enables him to reveal the obscured factors that could be causing a person to suffer from type 2 diabetes and hypothyroidism.