Diabetes and Alcohol: A Risky Combination

Diabetes and Alcohol: A Risky Combination
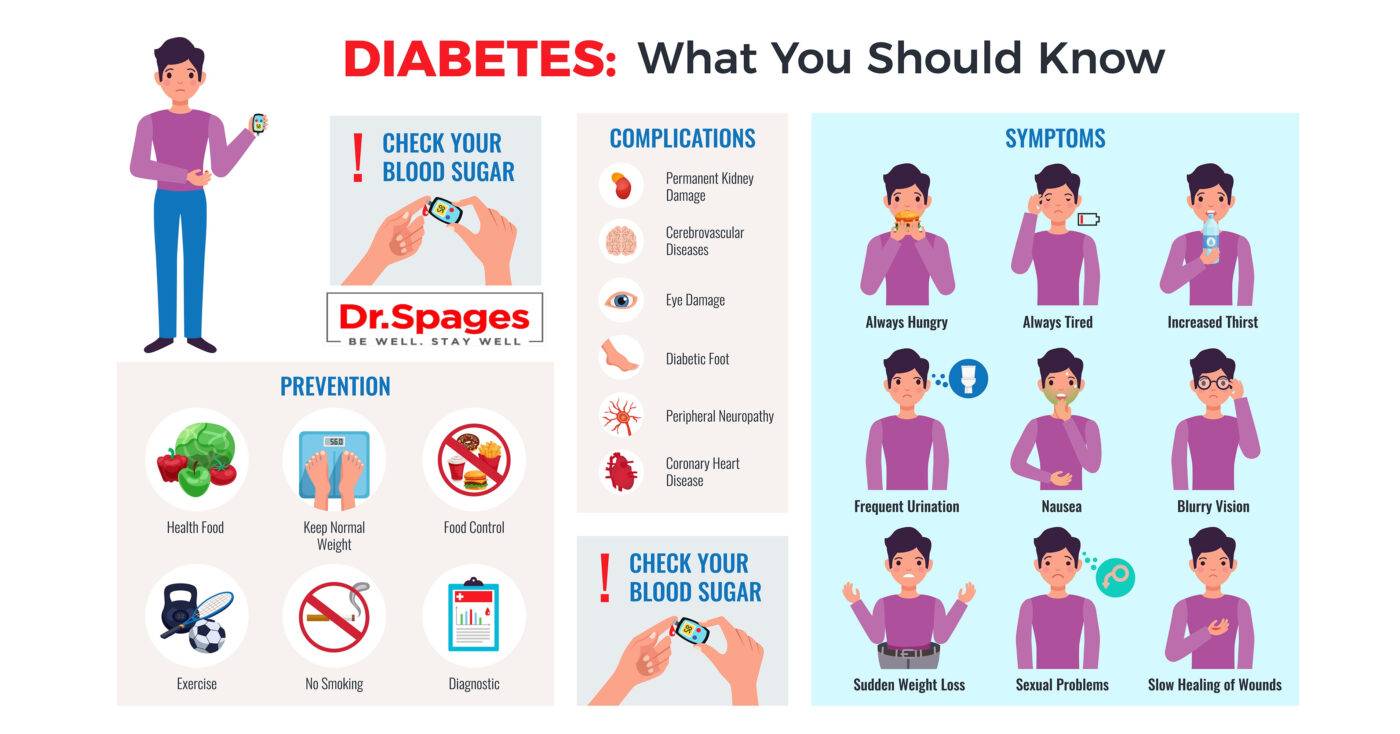
Diabetes is a long-term metabolic disorder characterized by high blood sugar levels. It affects millions of people globally and must be managed carefully to avoid problems. The usage of alcohol is one part of diabetes care that frequently creates issues and worries. While moderate alcohol intake can be part of a healthy lifestyle for some people, it poses special problems and risks for diabetics. We will delve into the complex relationship between diabetes and alcohol in this detailed guide, addressing the potential hazards, advantages, and practical suggestions for people living with this condition.
Understanding Diabetes
Before we explore the connection between diabetes and alcohol, it’s essential to have a basic understanding of diabetes itself. Diabetes is a group of diseases that affect how the body regulates blood sugar (glucose). The two most common types of diabetes are:
- Type 1 Diabetes: In this autoimmune condition, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, individuals with Type 1 diabetes require insulin therapy to survive. It typically develops in childhood or adolescence.
- Type 2 Diabetes: Type 2 diabetes is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin. Initially, the pancreas compensates by producing more insulin, but over time, it may fail to keep blood sugar levels in check. Type 2 diabetes is often associated with lifestyle factors such as obesity and physical inactivity, although genetics also play a role.
Diabetes and Blood Sugar Regulation
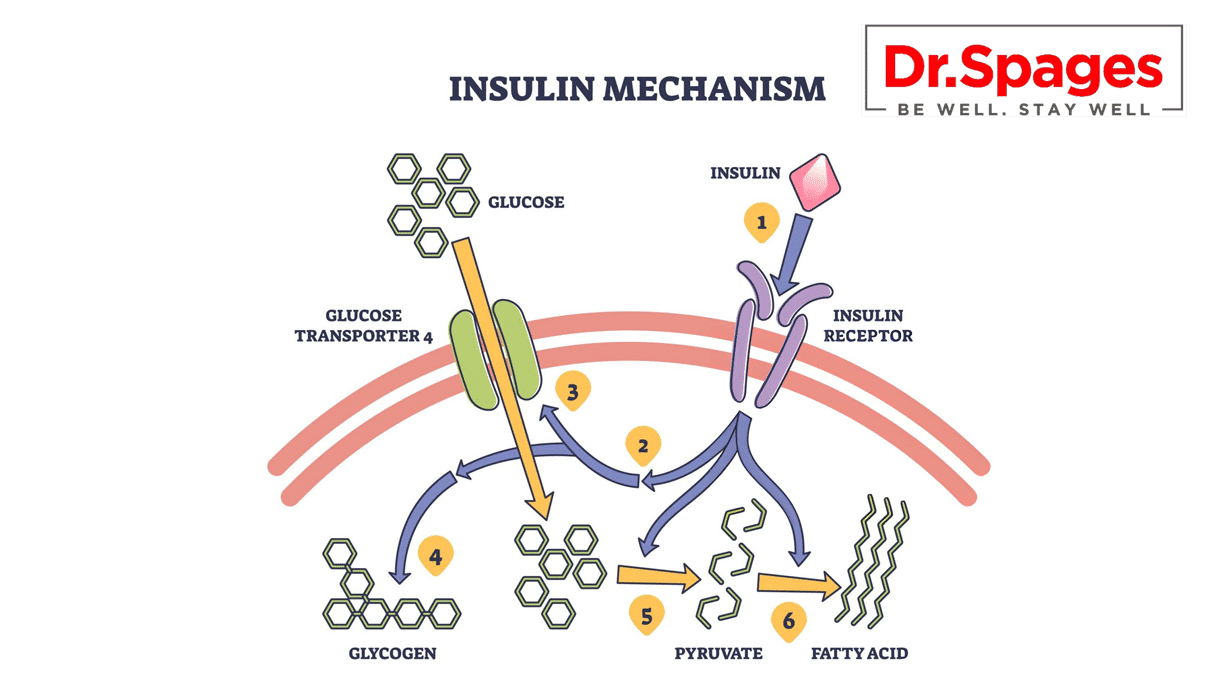
One of the primary concerns for individuals with diabetes is maintaining stable blood sugar levels. Blood sugar levels can be influenced by various factors, including diet, physical activity, medication, and stress. The role of insulin is central to this process:
– Insulin: Produced by the pancreas, insulin is a hormone that helps regulate blood sugar levels. It allows glucose to enter cells, where it can be used for energy or stored for future use.
For people with diabetes, this delicate balance is disrupted:
- Type 1 Diabetes: Individuals with Type 1 diabetes do not produce insulin and must receive it through injections or an insulin pump.
- Type 2 Diabetes: In Type 2 diabetes, insulin resistance means that cells do not respond effectively to insulin. The pancreas may produce more insulin to compensate, but over time, it may not be sufficient.
Alcohol and Its Impact on Blood Sugar
Now, let’s examine how alcohol consumption can affect blood sugar levels in individuals with diabetes:
- Immediate Impact:
Alcohol can have an immediate effect on blood sugar levels, depending on various factors, including the type and amount of alcohol consumed, whether it’s consumed with food, and an individual’s overall health.
- Hypoglycemia (Low Blood Sugar): Alcohol can lead to hypoglycemia, or low blood sugar, especially if it is consumed on an empty stomach. This is because alcohol can inhibit the liver from releasing stored glucose into the bloodstream. For individuals taking insulin or certain diabetes medications, this can be a significant concern.
- Delayed Impact:
The impact of alcohol on blood sugar levels may be delayed and more prolonged in some cases.
- Hyperglycemia (High Blood Sugar): While alcohol itself does not contain carbohydrates, many alcoholic beverages are mixed with sugary mixers or consumed alongside high-carb snacks. These additional carbohydrates can lead to elevated blood sugar levels hours after alcohol consumption.
- Alcohol and Medications:
Alcohol can interact with various diabetes medications, potentially increasing the risk of hypoglycemia.
- Oral Medications: Some diabetes medications, such as sulfonylureas (e.g., glyburide, glipizide), stimulate insulin production by the pancreas. When combined with alcohol, these medications can increase the risk of hypoglycemia.
- Insulin: Alcohol can affect the way the liver metabolizes insulin, potentially leading to unpredictable changes in blood sugar levels.
Risks and Considerations
- Hypoglycemia:
One of the most significant risks associated with alcohol consumption for individuals with diabetes is hypoglycemia, or low blood sugar. Symptoms of hypoglycemia can vary but often include:
- Shakiness
- Sweating
- Dizziness
- Confusion
- Rapid heartbeat
- Irritability
- Weakness
- Seizures (in severe cases)
- Loss of consciousness (in severe cases)
Hypoglycemia can be dangerous and even life-threatening if not promptly treated. Alcohol’s impact on blood sugar can make it challenging to recognize and manage hypoglycemia.
- Hyperglycemia:
While hypoglycemia is a primary concern, alcohol can also contribute to hyperglycemia, or high blood sugar, especially when consumed with sugary mixers or snacks. This delayed impact can make it difficult to manage blood sugar levels effectively.
- Impaired Judgment:
Alcohol can impair judgment and decision-making, which can lead to poor dietary choices and a lack of attention to blood sugar management.
- Medication Interactions:
Certain diabetes medications can interact with alcohol, amplifying its impact on blood sugar levels and increasing the risk of hypoglycemia. These interactions can vary depending on the specific medication.
- Increased Appetite:
Alcohol can stimulate appetite and lead to overeating, which can result in elevated blood sugar levels.
- Dehydration:
Alcohol is a diuretic, meaning it can lead to increased urination and dehydration. Dehydration can affect blood sugar control and increase the risk of hypoglycemia.
- Long-Term Health Risks:
Regular and excessive alcohol consumption is associated with several long-term health risks, including liver disease, cardiovascular problems, and nerve damage. These risks can compound the already heightened health concerns for individuals with diabetes.
Guidelines for Alcohol Consumption with Diabetes
Managing alcohol consumption when you have diabetes requires careful consideration and adherence to certain guidelines to minimize risks:
- Consult Your Healthcare Provider:
Before making any changes to your alcohol consumption, consult your healthcare provider. They can provide personalized guidance based on your specific diabetes management plan and medications.
- Limit Alcohol Intake:
Moderation is key. If you choose to consume alcohol, do so in moderation. Guidelines for moderate alcohol consumption typically include up to one drink per day for women and up to two drinks per day for men. A standard drink is defined as:
- – 12 ounces of beer (with about 5% alcohol content)
- – 5 ounces of wine (with about 12% alcohol content)
- – 1.5 ounces of distilled spirits (with about 40% alcohol content)
- Choose Wisely:
Opt for lower-carb and lower-sugar alcoholic beverages whenever possible. Dry wines, light beer, and distilled spirits with calorie-free mixers are generally better choices for blood sugar management.
- Eat When Drinking:
Never consume alcohol on an empty stomach. Eating a balanced meal or snack before drinking can help mitigate the risk of hypoglycemia.
- Monitor Blood Sugar:
Frequent monitoring of blood sugar levels is essential when consuming alcohol. This allows you to recognize and address any fluctuations promptly.
- Know Your Medications:
Understand how your diabetes medications interact with alcohol. Some medications, such as sulfonylureas and insulin, can increase the risk of hypoglycemia when combined with alcohol.
- Stay Hydrated:
Counteract the diuretic effects of alcohol by drinking plenty of water. Dehydration can exacerbate blood sugar fluctuations.
- Plan for Safety:
If you take insulin or medications that can cause hypoglycemia, inform a friend or family member about your diabetes and let them know how to recognize and respond to hypoglycemic episodes.
- Avoid Binge Drinking:
Binge drinking is associated with severe blood sugar fluctuations and other health risks. Stick to moderate, responsible drinking habits.
- Be Mindful of Mixers:
Many alcoholic beverages are mixed with high-sugar sodas or juices. Choose mixers that are lower in sugar or opt for sugar-free alternatives.
18 Best Salad Dressings for Type II Diabetics Ebook by Dr Spages
Incorporating salad into a balanced diet is unquestionably a smart choice for promoting good health. Unfortunately, most ready-made salad dressings available in stores are packed with excessive sugar, additives, and flavoured syrups, which can diminish the potential health benefits of your salad. Crafting your homemade salad dressing is a straightforward and cost-effective alternative to store-bought options. It also allows you to maintain greater control over the ingredients you’re using in your meals. Dr. Spages has put together a selection of homemade salad dressing recipes that are not only speedy and uncomplicated but also health-conscious.
Conclusion
Diabetes and alcohol have a complicated interaction, with both immediate and delayed impacts on blood sugar levels. While moderate alcohol intake may be tolerated by some diabetics, it requires careful evaluation, monitoring, and adherence to recommendations to reduce dangers.
Consult your healthcare professional if you have diabetes and are unclear whether alcohol can be a part of your lifestyle. They can offer tailored advice and assist you in making informed decisions that are consistent with your diabetes management strategy and overall health objectives. Remember that moderation, awareness, and proactive monitoring of your blood sugar levels are the keys to safe alcohol use with diabetes.
Please Note: The diet and watching carbs DOES NOT fix the root issues that make blood
sugar go up.