Exploring the Mechanisms of Beta Cell Regeneration for Diabetes Reversal
Beta Cell Regeneration for Diabetes Reversalillustration
Exploring the Mechanisms of Beta Cell Regeneration for Diabetes Reversal
Diabetes is a chronic disease characterized by hyperglycemia, which results from defects in insulin secretion and/or action. The prevalence of diabetes is increasing worldwide, with an estimated 463 million people living with the disease in 2019. Despite advances in the management of diabetes, there is still a need for effective treatments that can reverse the disease.
Beta cells are the cells in the pancreas that produce and secrete insulin. In type 1 diabetes, the immune system attacks and destroys beta cells, leading to a complete lack of insulin. In type 2 diabetes, beta cells become dysfunctional and are unable to secrete enough insulin to maintain normal blood glucose levels. One potential approach for diabetes reversal is the regeneration of beta cells. In this article, we will explore the mechanisms of beta cell regeneration and their potential for diabetes reversal.
Mechanisms of Beta Cell Regeneration
Beta cell regeneration can occur through several mechanisms, including replication of existing beta cells, differentiation of progenitor cells, and transdifferentiation of other cell types into beta cells.
Replication of Existing Beta Cells
In adults, beta cells have a low rate of replication under normal conditions. However, in response to certain stimuli, such as injury or increased demand for insulin, beta cells can replicate to increase their numbers. The molecular mechanisms that regulate beta cell replication are complex and not fully understood, but several signaling pathways have been implicated.
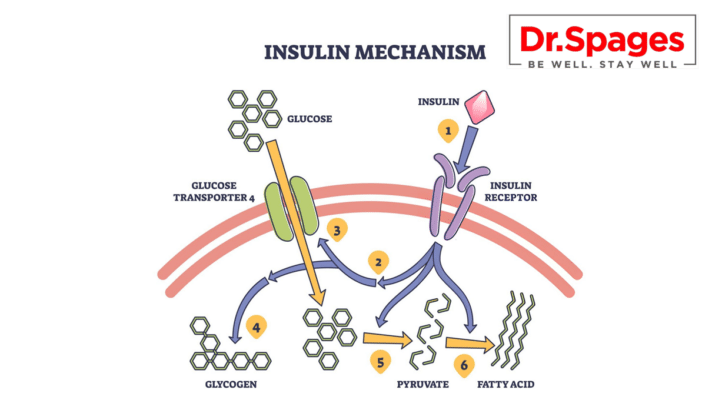
One key pathway involved in beta cell replication is the insulin/insulin-like growth factor (IGF) signaling pathway. Activation of this pathway promotes beta cell growth and survival, as well as insulin secretion. Another pathway involved in beta cell replication is the Wnt signaling pathway. Wnt signaling has been shown to promote beta cell proliferation and differentiation in vitro and in vivo.
Differentiation of Progenitor Cells
Progenitor cells are immature cells that have the potential to differentiate into specific cell types. In the pancreas, there are several types of progenitor cells that can differentiate into beta cells, including pancreatic ductal cells, acinar cells, and alpha cells.
One potential approach for beta cell regeneration is the differentiation of progenitor cells into beta cells. This approach has been shown to be effective in animal models of diabetes, but the mechanisms involved in the differentiation of progenitor cells into beta cells are not fully understood.
Transdifferentiation of Other Cell Types
Transdifferentiation is the process by which one cell type is converted into another cell type. In the pancreas, several cell types have been shown to be capable of transdifferentiating into beta cells, including alpha cells, delta cells, and pancreatic ductal cells.
Alpha cells are responsible for producing glucagon, a hormone that raises blood glucose levels. In response to certain stimuli, such as pancreatic injury or inhibition of glucagon signaling, alpha cells can transdifferentiate into beta cells. Delta cells, which produce somatostatin, have also been shown to transdifferentiate into beta cells in response to injury or loss of beta cells. Pancreatic ductal cells, which line the pancreatic ducts, have been shown to differentiate into beta cells in vitro and in vivo.
Potential for Diabetes Reversal
Beta cell regeneration has the potential to reverse diabetes by restoring the ability of the pancreas to produce and secrete insulin. Several approaches to beta cell regeneration have shown promise in preclinical and clinical studies.
One approach involves the use of small molecules or growth factors to promote beta cell replication or differentiation. For example, a study in mice showed that treatment with the small molecule harmine promoted beta cell replication and improved glucose tolerance. Similarly, treatment with the growth factors betacellulin and gastrin has been shown to promote beta cell proliferation and differentiation in vitro and in vivo.
Another approach involves the transplantation of progenitor cells or beta cells into the
pancreas. This approach has been successfully used in preclinical and clinical studies, but it is limited by the availability of donor cells and the risk of rejection by the recipient’s immune system.
Transdifferentiation of other cell types into beta cells also holds promise for diabetes reversal but it is incomplete. In animal models, transdifferentiation of alpha cells into beta cells has been shown to be effective in reversing diabetes. However, this approach is still in the early stages of research and has not yet been tested in humans.
Challenges and Future Directions
Despite the potential of beta cell regeneration for diabetes reversal, there are several challenges that must be overcome before this approach can be widely used in clinical practice.
One major challenge is identifying the optimal approach for beta cell regeneration. Different approaches may be more effective in different patients, depending on factors such as the extent of beta cell loss and the presence of underlying comorbidities.
Another challenge is ensuring the safety and efficacy of beta cell regeneration therapies. Some approaches, such as the transplantation of donor cells, carry a risk of rejection by the recipient’s immune system. Other approaches, such as the use of growth factors or small molecules, may have off-target effects or limited efficacy.
In the future, advances in stem cell research and gene editing technology may lead to new approaches for beta cell regeneration. For example, induced pluripotent stem cells (iPSCs) have the potential to differentiate into beta cells and may be used to produce an unlimited supply of donor cells for transplantation. Gene editing techniques, such as CRISPR/Cas9, may be used to modify progenitor cells or other cell types to differentiate into beta cells.
Conclusion
Beta cell regeneration holds promise as a potential approach for diabetes reversal however there are other organs and factors that should be explored. Several mechanisms of beta cell regeneration have been identified, including replication of existing beta cells, differentiation of progenitor cells, and transdifferentiation of other cell types into beta cells. Despite the potential of beta cell regeneration, there are several challenges that must be overcome before this approach can be widely used in clinical practice. Advances in stem cell research and gene editing technology may lead to new approaches for beta cell regeneration in the future. The best approach it to get to the root imbalances and to fix those with a comprehensive plan.
About Dr Spages
Dr. Spages is committed to providing customized healthcare services to individuals who have diabetes and women who are dealing with hypothyroidism. He takes pride in creating an atmosphere that is conducive to the recovery and motivation of his patients.
Dr. Jonathan Spages, DC is a Functional Medicine specialist with extensive knowledge and expertise in treating chronic health conditions such as type II diabetes and hypothyroidism. Unlike the conventional approach of primarily using medications and hormones, he uses advanced diagnostic testing and analysis methods to uncover the underlying causes of these conditions that are typically ignored in traditional medical settings.